How electronic claims work
Electronic claims are a method of submitting healthcare claims to insurance companies or payers electronically, rather than through traditional paper-based methods. Electronic claims are important for billing insurance because they offer several advantages over traditional paper-based claims.
Why are they important for billing insurance?
Here’s an overview of some of the key advantages:
-
Speed: Electronic claims can be submitted to insurance companies almost instantly, which can help speed up the payment process. This means that providers can receive payment more quickly and keep their practices running smoothly.
-
Accuracy: Electronic claims are less likely to contain errors or omissions, such as missing information or incorrect codes. This can help prevent delays in payment and reduce the need for resubmissions.
-
Efficiency: Electronic claims can help streamline the billing process for both providers and payers. With electronic claims, providers can submit claims electronically and receive payments electronically, which can help reduce the amount of paperwork and administrative tasks involved in the billing process. For payers, electronic claims can help reduce the amount of time and resources required to process claims and issue payments. By using electronic claims, you may also receive up-to-date claim status so you don’t have to contact the payer before ERAs are received.
-
Cost savings: Using electronic claims can help reduce the costs associated with processing and submitting paper-based claims. By adopting electronic claims, providers and payers can save money on printing, postage, and other administrative expenses.
-
Improved patient care: Electronic claims can help improve the overall quality of healthcare services by reducing the time and resources required for administrative tasks. This can free up more time for providers to focus on patient care and improve the patient experience.
The basics of electronic claims
Who are the different parties involved in the process?
The electronic claims process involves several parties, including healthcare providers and payers. Here’s a brief overview of each party’s role in the process:
-
Healthcare providers: Healthcare providers are the entities that provide medical services to patients, such as hospitals, physicians, and other medical professionals. Providers use electronic claims to submit billing information to insurance companies or payers for the services they provide. In the case of mental/behavioral health, the provider is the psychotherapist.
-
Insurance companies/payers: Insurance companies or payers are the entities responsible for paying healthcare providers for the services they provide to patients. Insurance companies receive electronic claims from healthcare providers and review them to determine if the services provided are covered under the patient’s insurance plan. If the services are covered, the insurance company will issue payment to the healthcare provider.
-
Billing software providers: Billing software providers are companies that provide healthcare providers with software tools to create and manage electronic claims. These software tools typically include features such as claim validation, claim submission, and payment posting. Sessions Health can be used as the billing software provider for submitting electronic claims.
-
Clearinghouses: Clearinghouses are companies that act as intermediaries between healthcare providers and insurance companies. Clearinghouses receive electronic claims from healthcare providers and transmit them to insurance companies or payers using standard formats and protocols. Clearinghouses also provide services such as claim validation and payment posting. Sessions Health connects to a clearinghouse to validate electronic claims.
-
Patients: Patients are the individuals who receive medical services from healthcare providers. Patients may be responsible for paying a portion of the cost of their medical services, depending on their insurance coverage.
Overall, the electronic claims process involves multiple parties working together to ensure that healthcare providers are paid for the services they provide to patients.
The details of electronic claims and how they work
Electronic claims, also known as electronic data interchange (EDI) claims, can include information such as patient demographics, medical codes, diagnoses, and treatment information. Electronic claims typically use standard electronic formats, such as the ANSI X12 837 format, to ensure that the information is easily readable and understandable by insurance companies or payers. The format includes various segments, such as header segments, service line segments, and footer segments, that organize the information in a structured way.
Electronic claims work by using specialized software or services to transmit the claim information from the provider’s billing system to the insurance company or payer’s system. The process typically involves several steps:
-
The provider submits the claim electronically using their billing software or a specialized service provider.
-
The claim is validated to ensure that it meets the necessary formatting and content requirements.
-
The claim is transmitted securely to the insurance company or payer’s system using a standard protocol, such as electronic data interchange (EDI).
-
The insurance company or payer’s system receives the claim, processes it, and determines whether to approve or deny the claim.
-
If the claim is approved, payment is issued electronically to the provider’s bank account.
-
Remittance (information about the payment) is sent back to the EHR from the payer.
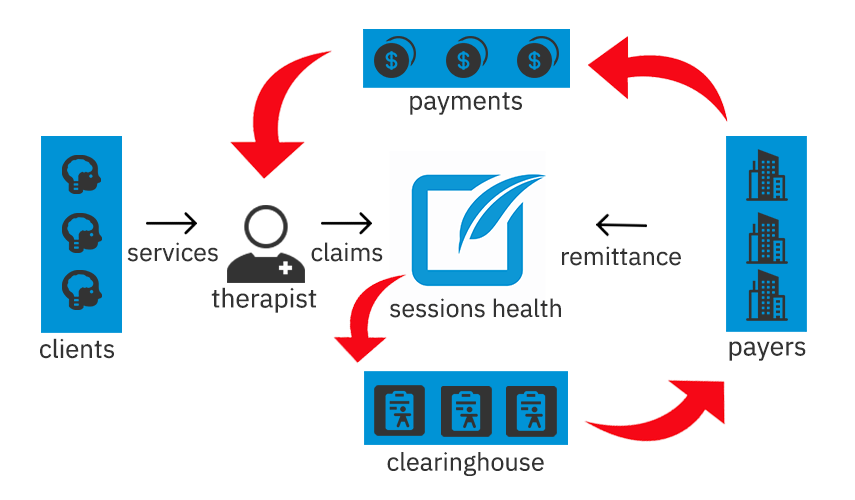
Sessions Health is a behavioral health EHR that coordinates sending and receiving electronic claims data
By using standard electronic formats and secure transmission protocols, electronic claims help ensure that the information is accurate, complete, and easily understandable by all parties involved.
What are the different types of EDI transactions, such as 837 and 835?
There are several different types of EDI transactions that are commonly used in the healthcare industry. Two of the most important ones that relate to electronic claims are the 837 and 835 formats.
-
837: The 837 format is used to submit electronic claims to insurance companies or payers. The 837 format includes several segments, such as the header, patient, provider, diagnosis, and service line segments. The header segment includes information such as the claim number, date of service, and provider information. The patient segment includes information such as the patient’s name, address, and insurance information. The provider segment includes information about the healthcare provider submitting the claim, such as their name, address, and National Provider Identifier (NPI) number. The diagnosis segment includes information about the patient’s medical diagnosis, while the service line segment includes information about the specific services provided and associated charges.
-
835: The 835 format is used to receive electronic remittance advice (ERA) from insurance companies or payers. The 835 format includes several segments, such as the header, provider, claim payment, and adjustment segments. The header segment includes information such as the provider’s name, address, and NPI number. The provider segment includes information about the healthcare provider receiving the payment. The claim payment segment includes information about the specific claims being paid, including the amount paid and any adjustments made. The adjustment segment includes information about any adjustments made to the payment, such as denials or partial payments.
Other types of EDI transactions include the 270/271 format, which is used to check patient eligibility and benefits, and the 276/277 format, which is used to submit and receive requests for healthcare services and responses to those requests.
Overall, understanding the different types of EDI transactions used in conjunction with electronic claims is important for healthcare providers and payers, as it can help ensure that claims are submitted and processed accurately and efficiently.
Electronic claims and healthcare technology
How electronic claims fit into the larger context of healthcare technology
Electronic claims are one of the many technologies that are transforming the healthcare industry. Electronic health records (EHRs) and telehealth are two other technologies that are playing an increasingly important role in the delivery of healthcare services. Here’s how electronic claims fit into the larger context of healthcare technology:
-
Integration with EHRs: Electronic claims are often integrated with electronic health records (EHRs) systems, allowing providers to easily access patient information and submit claims for reimbursement. This integration can help reduce errors and improve accuracy, since the claims data can be automatically populated with information from the patient’s EHR. Sessions Health is an EHR that can transmit your electronic claims.
-
Telehealth: Telehealth, or the delivery of healthcare services remotely using technology, is becoming increasingly popular. Electronic claims can be used to submit claims for telehealth services, allowing providers to receive reimbursement for these services without having to submit paper claims.
-
Interoperability: The healthcare industry is increasingly focused on improving interoperability, or the ability of different technology systems to communicate with each other. Electronic claims are a key part of this effort, since they rely on standardized codes and formats that can be easily shared between different systems.
-
Analytics: Healthcare organizations are increasingly using analytics tools to analyze data and identify trends and opportunities for process improvement. Electronic claims can provide a wealth of data that can be analyzed to identify opportunities for cost savings, process improvement, and other initiatives.
Overall, electronic claims are just one piece of a larger puzzle in the healthcare technology landscape. As the industry continues to evolve and embrace new technologies, electronic claims will remain an important part of the claims and reimbursement process. By integrating with EHRs, supporting telehealth, promoting interoperability, and providing valuable data for analytics, electronic claims will continue to play a key role in the delivery of healthcare services.
Conclusion
Call-to-action for providers to adopt electronic claims
As healthcare technology continues to advance, the adoption of electronic claims is becoming increasingly important for providers such as mental health professionals. By transitioning to electronic claims systems, therapists can improve their efficiency, reduce errors, and ultimately provide better care to their patients.
If you are a mental health professional, it is important to evaluate your current billing processes and consider the benefits of transitioning to electronic claims. By doing so, you can improve your cash flow, reduce administrative burden, and free up resources to focus on providing high-quality care to your patients.
Don’t let outdated billing processes hold you back from providing the best care possible. Take action today to explore the benefits of electronic claims and integrate them into your healthcare technology strategy.